















Neurologic involvement is common in individuals with mucopolysaccharidosis (MPS) and may constitute some of the first presenting symptoms of disease. It is important for neurology to consider MPS in a variety of presentations, as patterns of neurologic involvement vary substantially by MPS subtype. MPS may present with or without intellectual disability and, for some subtypes, central nervous system involvement is primarily due to cervical spinal subluxation and cord compression.1-3
Along with these common neurologic signs and symptoms, the following should also raise your index of suspicion for MPS1:
Nuclear magnetic resonance image of a patient with MPS showing marked supratentorial hydrocephalus.
Courtesy of Dr Grimaldi M. and Dr Parini R. (Monza).
Nuclear magnetic resonance image of the craniocervical junction with the head in neutral position (left) and with flexion of the head towards the neck (right), showing reduction in the diameter of the vertebral canal at the craniocervical junction with consequent compression of the spinal cord.
Courtesy of Dr Grimaldi M. and Dr Parini R. (Monza).
Respiratory symptoms are commonly seen in individuals with mucopolysaccharidosis (MPS) and may lead to an MPS diagnosis. Airway obstruction and respiratory impairment are prominent features of MPS and may progress early in the course of the disease.1
Respiratory disorders are prevalent across most MPS types and have a variety of manifestations, including narrow airways and sleep-disordered breathing.2
Along with these common respiratory signs, the following should also raise your index of suspicion for MPS:
Radiograph image of the anteroposterior chest in an 11-year-old female patient with MPS VI showing thick but not paddle-shaped ribs and thick clavicles.
Source: Skeletal Radiology, volume 43, issue 3. Lachman RS, Burton BK, Clarke LA, Hoffinger S, Ikegawa S, Jin D-K, Kano H, Kim O-H, Lampe C, Mendelsohn NJ, Shediac R, Tanpaiboon P, White KK. Mucopolysaccharidosis IVA (Morquio A syndrome) and VI (Maroteaux-Lamy syndrome): under-recognized and challenging to diagnose. Pages 359-369. Copyright (C) Lachman RS, Burton BK, Clarke LA, Hoffinger S, Ikegawa S, Jin D-K, Kano H, Kim O-H, Lampe C, Mendelsohn NJ, Shediac R, Tanpaiboon P, White KK 2014.
Multidetector computed tomography scans of the trachea in patients with MPS.
Courtesy of Dr Grimaldi M. and Dr Parini R. (Monza).
Ear, nose, and throat (ENT) manifestations are commonly seen in individuals with mucopolysaccharidosis (MPS) and are often among the first symptoms to appear. Common manifestations include but are not limited to adenotonsillar hypertrophy, frequent infections of the upper airway, and hearing loss.1,2
Any number of ENT symptoms, especially if coupled with other systemic signs and symptoms, should prompt referral to a geneticist or metabolic center.3,4 Along with the common ENT and respiratory signs, these additional features should also raise your index of suspicion for MPS5:
Computed tomography scan of the ear of a patient with MPS.
Courtesy of Dr Grimaldi M. and Dr Parini R. (Monza).
Ocular manifestations often arise prior to other features of mucopolysaccharidosis (MPS) and vary by type and severity among the MPS disorders. Corneal clouding is a hallmark feature of MPS.1
Ocular features—often leading to visual impairment—have been described in all types of MPS and should raise suspicion of MPS.
Common ocular manifestations include the following2:
Bone- and joint-related features are common from a very early stage of disease in patients with most types of mucopolysaccharidosis (MPS) disorders. Patients with these types of musculoskeletal manifestations often present to a rheumatologist—and often before MPS is diagnosed.1
Rheumatologic involvement is uniformly progressive, with incidence and severity increasing over time. Although patients with MPS typically present with a wide range or cluster of symptoms, isolated symptoms may be sufficient to merit referral to a geneticist or metabolic center.1,2
Signs and symptoms may be subtle or overt. Common bone and joint features suggestive of MPS include the following1:
Rheumatologists should additionally consider an MPS referral in patients with any of the following:
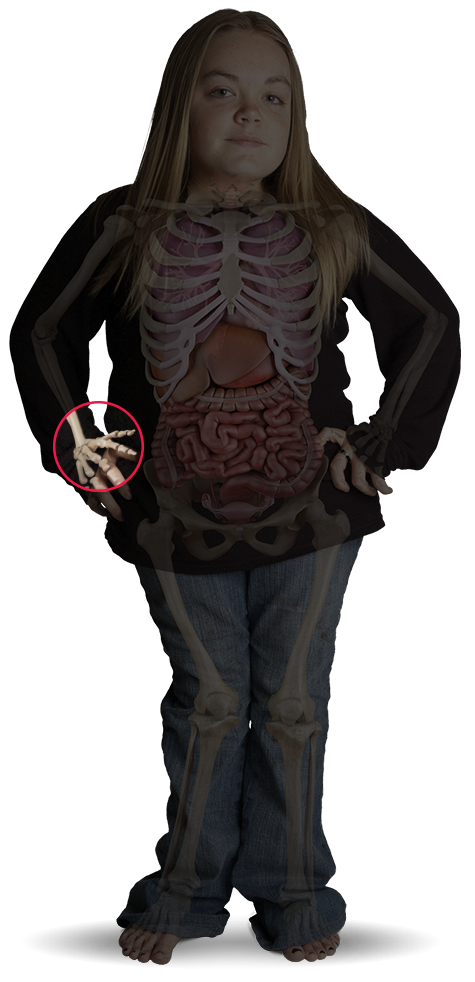
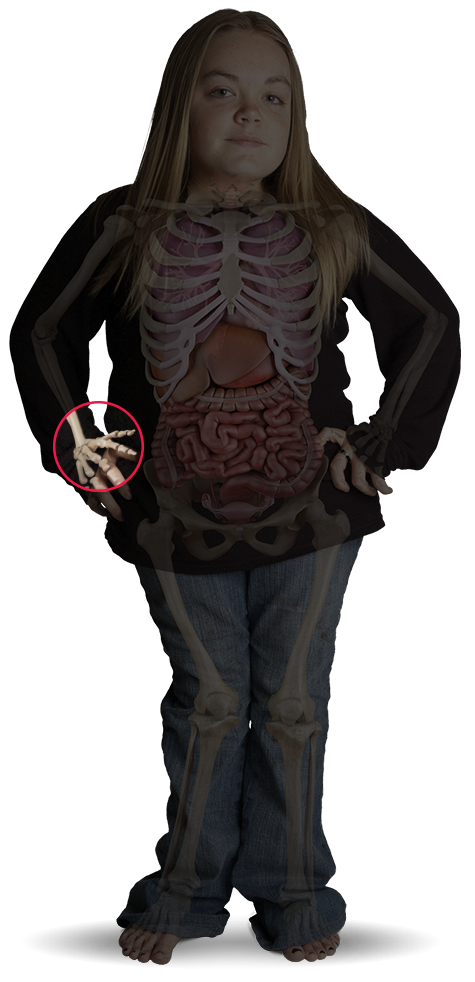
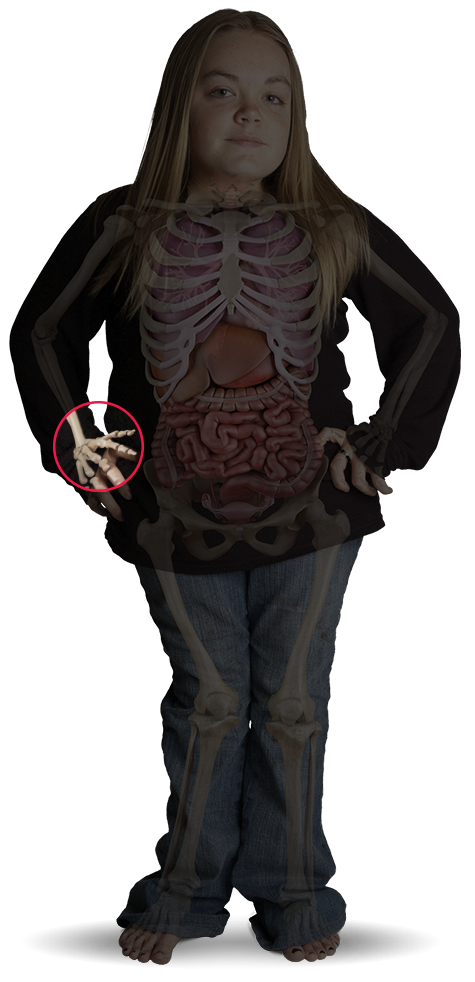
Manifestations of dysostosis multiplex in the hands. Radiograph showing hands of a patient with MPS in early childhood, with moderately severe proximal pointing and expanded metacarpals with thin cortices.
Reproduced with permission from Lachman, J Pediatr Rehabil Med, 2010.
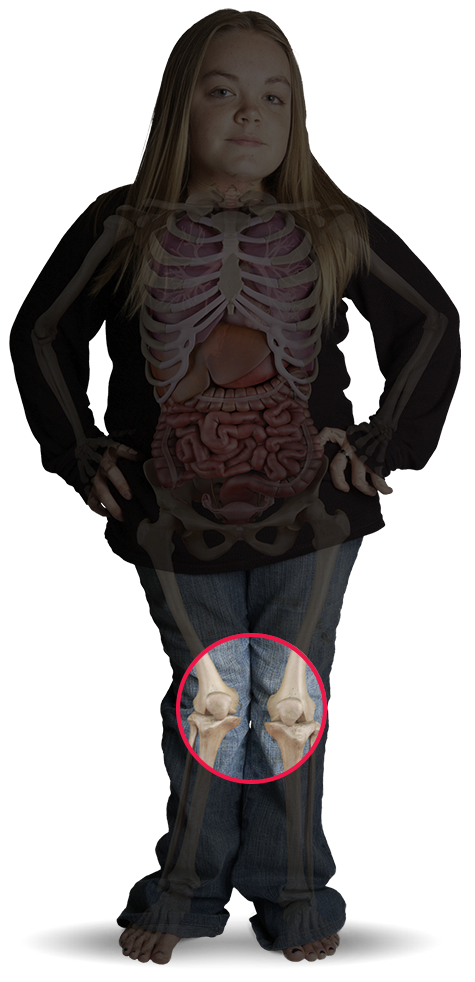
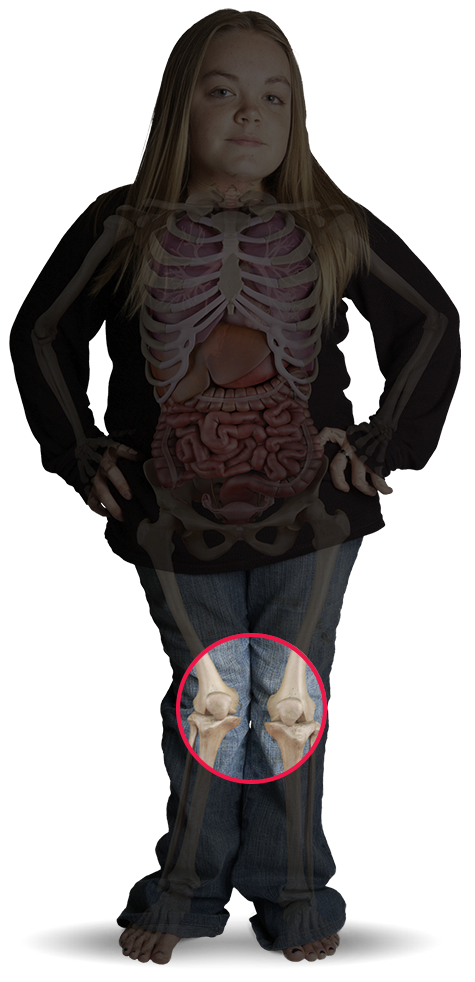
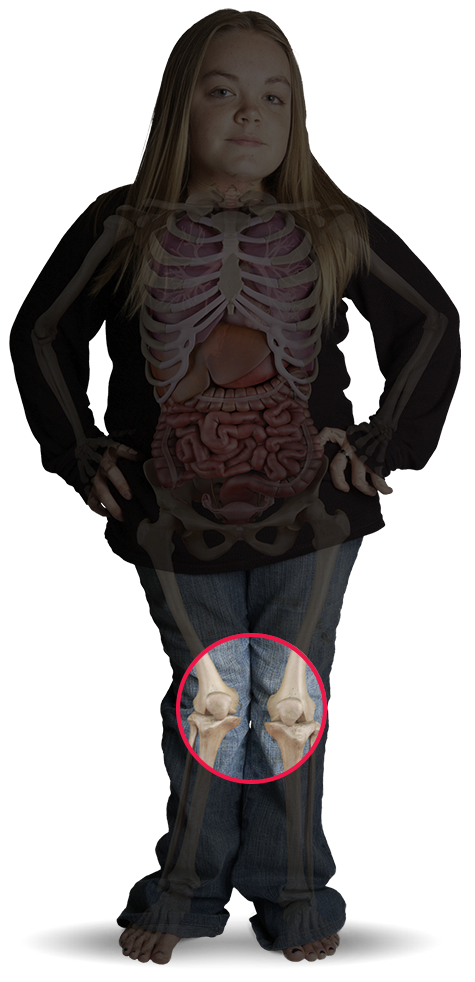
Radiograph of anteroposterior pelvis and hips in a 27-year-old patient with Morquio A showing mildly dysplastic capital femoral epiphysis with joint space narrowing and sclerosis (degenerative arthrosis).
Source: Skeletal Radiology, volume 43, issue 3. Lachman RS, Burton BK, Clarke LA, Hoffinger S, Ikegawa S, Jin D-K, Kano H, Kim O-H, Lampe C, Mendelsohn NJ, Shediac R, Tanpaiboon P, White KK. Mucopolysaccharidosis IVA (Morquio A syndrome) and VI (Maroteaux-Lamy syndrome): under-recognized and challenging to diagnose. Pages 359-369. Copyright (C) Lachman RS, Burton BK, Clarke LA, Hoffinger S, Ikegawa S, Jin D-K, Kano H, Kim O-H, Lampe C, Mendelsohn NJ, Shediac R, Tanpaiboon P, White KK 2014.
Cardiac involvement is commonly seen in individuals with mucopolysaccharidosis (MPS) and leads to extensive morbidity and, potentially, premature mortality. Early suspicion is therefore critical, regardless of whether cardiac symptoms are seen alone or in combination with other symptoms.1
The most common cardiac findings in MPS, as reported in an evaluation of 28 patients aged 2 to 14 years were1
Along with the preceding common cardiac signs, the following signs should raise your index of suspicion for MPS:
Courtesy of Dr Russo P. and Dr Parini R. (Monza).
Courtesy of Dr Russo P. and Dr Parini R. (Monza).
Classically, mucopolysaccharidosis (MPS) is associated with a cluster of signs and symptoms referred to as dysostosis multiplex, with the exception of MPS III. However, recognition of early and nonclassic skeletal symptoms prior to more robust skeletal progression can enable early recognition, and should prompt referral to a geneticist or metabolic center.1
Most MPS types are characterized by skeletal abnormalities and joint disease with hallmark features of dysostosis multiplex.1,2
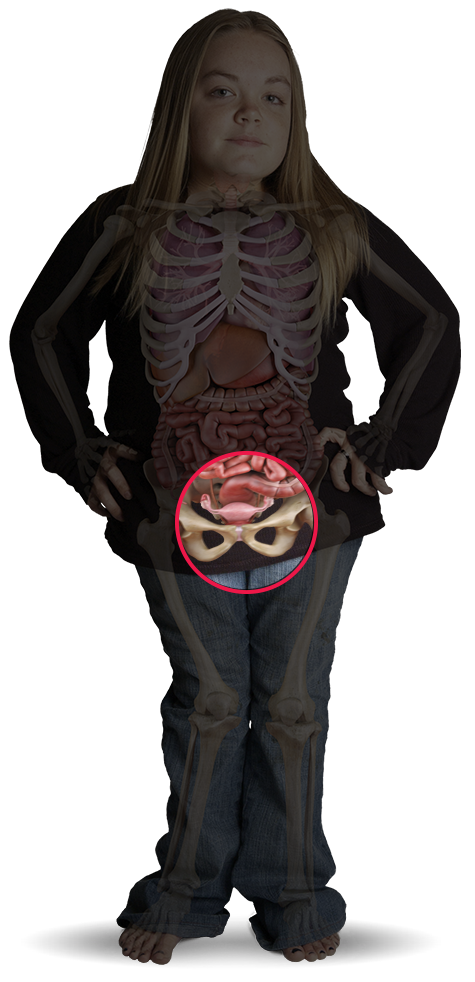
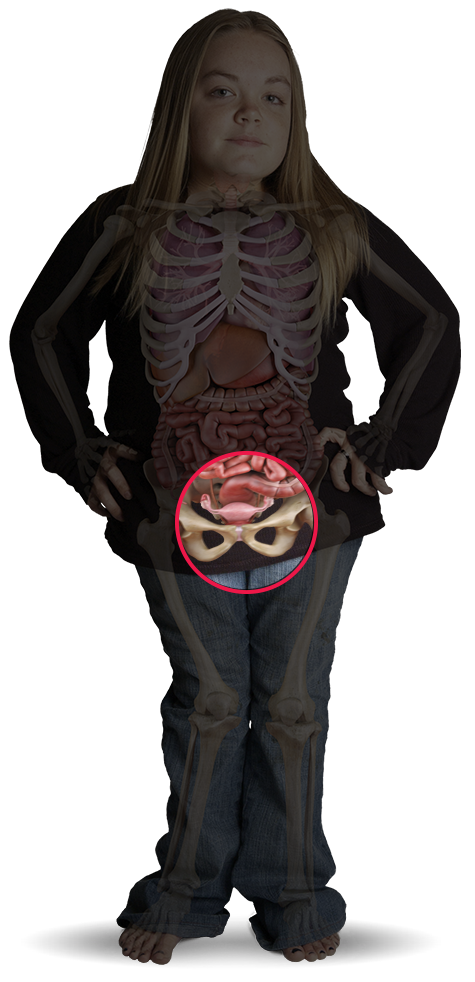
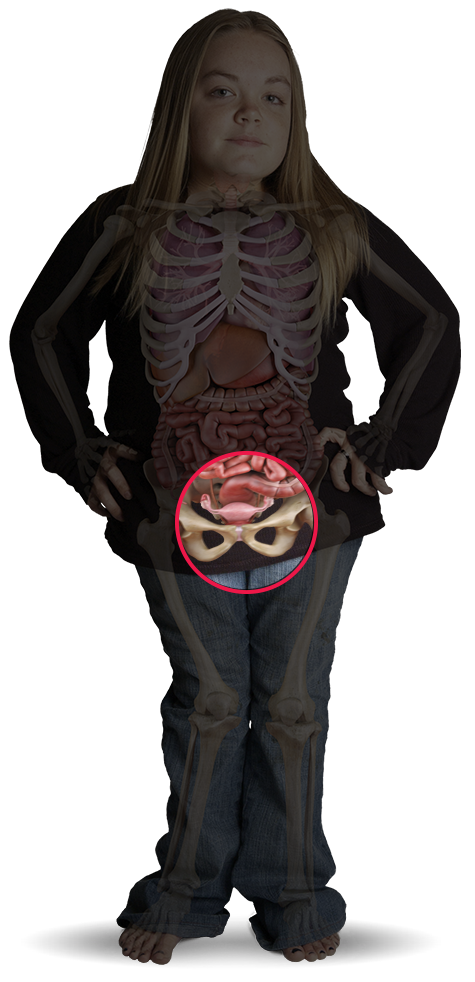
Radiograph image showing dysostosis multiplex manifestations in the pelvis and hips of a patient with MPS. Rounded iliac wings, double-contoured ileal lateral walls (arrows), and elongated femoral necks.
Reproduced with permission from Lachman, J Pediatr Rehabil Med, 2010.
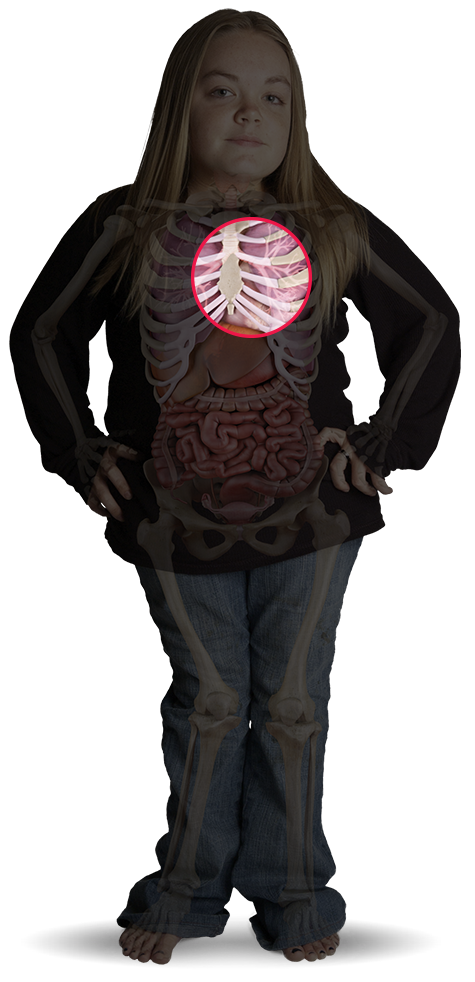
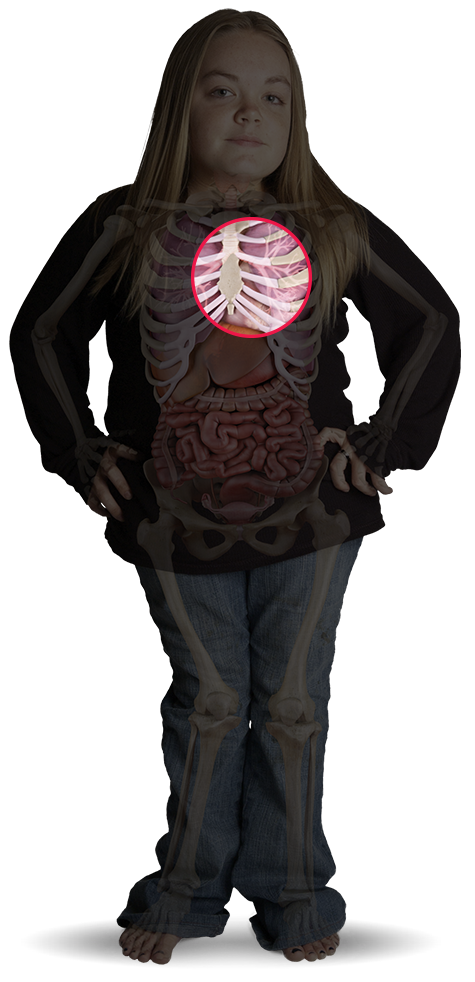
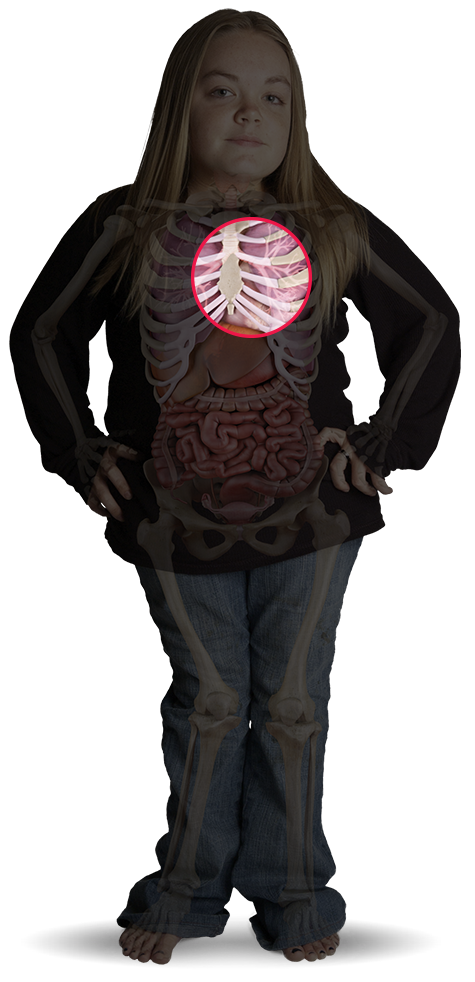
Radiograph of the chest of a patient with MPS showing paddle-shaped ribs and short thickened clavicles (arrows).
Reproduced with permission from Lachman, J Pediatr Rehabil Med, 2010.
Radiograph of anteroposterior pelvis and hips in a 27-year-old patient with Morquio A showing mildly displastic capital femoral epiphysis with joint space narrowing and sclerosis (degenerative arthrosis).
Source: Skeletal Radiology, volume 43, issue 3. Lachman RS, Burton BK, Clarke LA, Hoffinger S, Ikegawa S, Jin D-K, Kano H, Kim O-H, Lampe C, Mendelsohn NJ, Shediac R, Tanpaiboon P, White KK. Mucopolysaccharidosis IVA (Morquio A syndrome) and VI (Maroteaux-Lamy syndrome): under-recognized and challenging to diagnose. Pages 359-369. Copyright (C) Lachman RS, Burton BK, Clarke LA, Hoffinger S, Ikegawa S, Jin D-K, Kano H, Kim O-H, Lampe C, Mendelsohn NJ, Shediac R, Tanpaiboon P, White KK 2014.
Regardless of the clinical setting, there are overt and generally observable signs that should raise your suspicion of mucopolysaccharidosis (MPS) disorders, including1-18
Consideration of MPS based on suspicious patterns of signs and symptoms is the first step to arriving at a definitive diagnosis of a specific MPS disorder. Of particular importance, recognition of the heterogeneous nature of slowly progressive disease is essential to reduce time to diagnosis for many patients.3
References: 1. Berger KI, Fagondes SC, Giugliani R, et al. Respiratory and sleep disorders in mucopolysaccharidosis. J Inherit Metab Dis. 2013;36(2):201-210. doi:10.1007/s10545-012-9555-1. 2. Mesolella M, Cimmino M, Cantone E, et al. Management of otolaryngological manifestations in mucopolysaccharidoses: our experience. Acta Otorhinolaryngol Ital. 2013;33(4):267-272. 3. Lehman TJA, Miller N, Norquist B, Underhill L, Keutzer J. Diagnosis of the mucopolysaccharidoses. Rheumatology. 2011;50(suppl 5):v41-v48. 4. Wood TC, Harvey K, Beck M, et al. Diagnosing mucopolysaccharidosis IVA. J Inherit Metab Dis. 2013;36(2):293-307. doi:10.1007/s10545-013-9587-1. 5. Muenzer J. Early initiation of enzyme replacement therapy for the mucopolysaccharidoses. Mol Genet Metab. 2014;111(2):63-72. doi:10.1016/j.ymgme.2013.11.015. 6. Hendriksz CJ, Al-Jawad M, Berger KI, et al. Clinical overview and treatment options for non-skeletal manifestations of mucopolysaccharidosis type IVA. J Inherit Metab Dis. 2013;36(2):309-322. doi:10.1007/s10545-012-9459-0. 7. Simmons MA, Bruce IA, Penney S, Wraith E, Rothera MP. Otorhinolaryngological manifestations of the mucopolysaccharidoses. Int J Pediatr Otorhinolaryngol. 2005;69(5):589-595. doi:10.1016/j.ijporl.2005.01.017.
References: 1. Muenzer J. The mucopolysaccharidoses: a heterogeneous group of disorders with variable pediatric presentations. J Pediatr. 2004;144(suppl 5):S27-S34. 2. Lachman RS, Burton BK, Clarke LA, et al. Mucopolysaccharidosis IVA (Morquio A syndrome) and VI (Maroteaux-Lamy syndrome): under-recognized and challenging to diagnose. Skeletal Radiol. 2014;43(3):359-369. doi:10.1007/s00256-013-1797-y. 3. Thümler A, Miebach E, Lampe C, et al. Clinical characteristics of adults with slowly progressing mucopolysaccharidosis VI: a case series. J Inherit Metab Dis. 2012;35(6):1071-1079. doi:10.1007/s10545-012-9474-1. 4. Montaño AM, Tomatsu S, Gottesman GS, Smith M, Orii T. International Morquio A Registry: clinical manifestation and natural course of Morquio A disease. J Inherit Metab Dis. 2007;30(2):165-174. doi:10.1007/s10545-007-0529-7. 5. Kinirons MJ, Nelson J. Dental findings in mucopolysaccharidosis type IV A (Morquio’s disease type A). Oral Surg Oral Med Oral Pathol. 1990;70(2):176-179. 6. Hendriksz CJ, Berger KI, Giugliani R, et al. International guidelines for the management and treatment of Morquio A syndrome. Am J Med Genet Part A. 2014;9999A:1-15. doi:10.1002/ajmg.a.36833. 7. Lachman R, Martin KW, Castro S, Basto MA, Adams A, Teles EL. Radiologic and neuroradiologic findings in the mucopolysaccharidoses. J Pediatr Rehabil Med. 2010;3(2):109-118. doi:10.3233/PRM-2010-0115. 8. Hendriksz C. Improved diagnostic procedures in attenuated mucopolysaccharidosis. Br J Hosp Med. 2011;72(2):91-95. 9. Cimaz R, Coppa GV, Koné-Paut I, et al. Joint contractures in the absence of inflammation may indicate mucopolysaccharidosis [hypothesis]. Pediatr Rheumatol Online J. 2009;7:18. doi:10.1186/1546-0096-7-18. 10. Fahnehjelm KT, Ashworth JL, Pitz S, et al. Clinical guidelines for diagnosing and managing ocular manifestations in children with mucopolysaccharidosis. Acta Ophthalmol. 2012;90(7):595-602. doi:10.1111/j.1755-3768.2011.02280.x. 11. Zafeiriou DI, Batzios SP. Brain and spinal MR imaging findings in mucopolysaccharidoses: a review. AJNR Am J Neuroradiol. 2013;34(1):5-13. doi:10.3174/ajnr.A2832. 12. Braunlin EA, Harmatz PR, Scarpa M, et al. Cardiac disease in patients with mucopolysaccharidosis: presentation, diagnosis and management. J Inherit Metab Dis. 2011;34(6):1183-1197. doi:10.1007/s10545-011-9359-8. 13. Braunlin E, Orchard PJ, Whitley CB, Schroeder L, Reed RC, Manivel JC. Unexpected coronary artery findings in mucopolysaccharidosis. Report of four cases and literature review. Cardiovasc Pathol. 2014;23(3):145-151. doi:10.1016/j.carpath.2014.01.001. 14. Mesolella M, Cimmino M, Cantone E, et al. Management of otolaryngological manifestations in mucopolysaccharidoses: our experience. Acta Otorhinolaryngol Ital. 2013;33(4):267-272. 15. Berger KI, Fagondes SC, Giugliani R, et al. Respiratory and sleep disorders in mucopolysaccharidosis. J Inherit Metab Dis. 2013;36(2):201-210. doi:10.1007/s10545-012-9555-1. 16. Lehman TJA, Miller N, Norquist B, Underhill L, Keutzer J. Diagnosis of the mucopolysaccharidoses. Rheumatology. 2011;50(suppl 5):v41-v48. 17. Martins AM, Dualibi AP, Norato D, et al. Guidelines for the management of mucopolysaccharidosis type I. J Pediatr. 2009;155(4)(suppl 2):S32-S46. doi:10.1016/j.jpeds.2009.07.005. 18. Clarke LA, Winchester B, Giugliani R, Tylki-Szymańska A, Amartino H. Biomarkers for the mucopolysaccharidoses: discovery and clinical utility. Mol Genet Metab. 2012;106(4):396-402. doi:10.1016/j.ymgme.2012.05.003.
References: 1. Lachman RS, Burton BK, Clarke LA, et al. Mucopolysaccharidosis IVA (Morquio A syndrome) and VI (Maroteaux-Lamy syndrome): under-recognized and challenging to diagnose. Skeletal Radiol. 2014;43(3):359-369. doi:10.1007/s00256-013-1797-y. 2. Lachman R, Martin KW, Castro S, Basto MA, Adams A, Teles EL. Radiologic and neuroradiologic findings in the mucopolysaccharidoses. J Pediatr Rehabil Med. 2010;3(2):109-118. doi:10.3233/PRM-2010-0115.
References: 1. Zafeiriou DI, Batzios SP. Brain and spinal MR imaging findings inmucopolysaccharidoses: a review. AJNR Am J Neuroradiol. 2013;34(1):5-13. doi:10.3174/ajnr.A2832. 2. Muenzer J. The mucopolysaccharidoses: a heterogeneous group of disorders with variable pediatric presentations. J Pediatr. 2004;144(suppl 5):S27-S34. 3. Solanki GA, Martin KW, Theroux MC, et al. Spinal involvement in mucopolysaccharidosis IVA (Morquio-Brailsford or Morquio A syndrome): presentation, diagnosis and management. J Inherit Metab Dis. 2013;36(2):339-355. doi:10.1007/s10545-013-9586-2. 4. White DA, Connor LT, Nardos B, et al. Age-related decline in the microstructural integrity of white matter in children with early- and continuously-treated PKU: A DTI study of the corpus callosum. 2010;99(suppl 1):S41-S46. doi:10.1016/j.ymgme.2009.09.016.
References: 1. Chiang J, Raiman J, Cutz E, Solomon M, Dell S. Tachypnea of infancy as the first sign of Sanfilippo syndrome. Pediatrics. 2014;134(3):e884-e888. doi:10.1542/peds.2013-2765. 2. Muhlebach MS, Wooten W, Muenzer J. Respiratory manifestations in mucopolysaccharidoses. Paediatr Respir Rev. 2011;12(2):133-138. doi:10.1016/j.prrv.2010.10.005. 3. Santamaria F, Andreucci MV, Parenti G, et al. Upper airway obstructive disease in mucopolysaccharidoses: polysomnography, computed tomography and nasal endoscopy findings. J Inherit Metab Dis. 2007;30(5):743-749. doi:10.1007/s10545-007-0555-5. 4. Berger KI, Fagondes SC, Giugliani R, et al. Respiratory and sleep disorders in mucopolysaccharidosis. J Inherit Metab Dis. 2013;36(2):201-210. doi:10.1007/s10545-012-9555-1.
References: 1. Lehman TJA, Miller N, Norquist B, Underhill L, Keutzer J. Diagnosis of the mucopolysaccharidoses. Rheumatology. 2011;50(suppl 5):v41-v48. 2. Wood T, Bodamer OA, Burin MG, et al. Expert recommendations for the laboratory diagnosis of MPS VI. Mol Genet Metab. 2012;106(1):73-82. doi:10.1016/j.ymgme.2012.02.005. 3. Cimaz R, Coppa GV, Koné-Paut I, et al. Joint contractures in the absence of inflammation may indicate mucopolysaccharidosis [hypothesis]. Pediatr Rheumatol Online J. 2009;7:18. doi:10.1186/1546-0096-7-18. 4. Muenzer J, Beck M, Eng CM, et al. Long-term, open-labeled extension study of idursulfase in the treatment of Hunter syndrome. Genet Med. 2011;13(2):95-101. doi:10.1097/GIM.0b013e3181fea459. 5. Hendriksz C. Improved diagnostic procedures in attenuated mucopolysaccharidosis. Br J Hosp Med. 2011;72(2):91-95. 6. Morishita K, Petty RE. Musculoskeletal manifestations of mucopolysaccharidoses. Rheumatology. 2011;50(suppl 5):v19-v25. doi:10.1093/rheumatology/ker397. 7. Solanki GA, Martin KW, Theroux MC, et al. Spinal involvement in mucopolysaccharidosis IVA (Morquio-Brailsford or Morquio A syndrome): presentation, diagnosis and management. J Inherit Metab Dis. 2013;36(2):339-355. doi:10.1007/s10545-013-9586-2.
References: 1. Ashworth JL, Kruse FE, Bachmann B, et al. Ocular manifestations in the mucopolysaccharidoses – a review. Clin Experiment Ophthalmol. 2010;38(suppl 1):12-22. doi:10.1111/j.1442-9071.2010.02364.x. 2. Fahnehjelm KT, Ashworth JL, Pitz S, et al. Clinical guidelines for diagnosing and managing ocular manifestations in children with mucopolysaccharidosis. Acta Ophthalmol. 2012;90(7):595-602. doi:10.1111/j.1755-3768.2011.02280.x.
References: 1. Braunlin EA, Harmatz PR, Scarpa M, et al. Cardiac disease in patients with mucopolysaccharidosis: presentation, diagnosis and management. J Inherit Metab Dis. 2011;34(6):1183-1197. doi:10.1007/s10545-011-9359-8. 2. Mohan UR, Hay AA, Cleary MA, Wraith JE, Patel RG. Cardiovascular changes in children with mucopolysaccharide disorders. Acta Paediatr. 2002;91(7):799-804. 3. Lachman R, Martin KW, Castro S, Basto MA, Adams A, Teles EL. Radiologic and neuroradiologic findings in the mucopolysaccharidoses. J Pediatr Rehabil Med. 2010;3(2):109-118. doi:10.3233/PRM-2010-0115. 4. Hendriksz C. Improved diagnostic procedures in attenuated mucopolysaccharidosis. Br J Hosp Med. 2011;72(2):91-95.